Value-based healthcare in the new workspace – resilience versus efficiency.
A New Workspace Guide - a new digitized workspace as well as self-determined work culture in the fight against the shortage of skilled nursing staff as well as collapse of health care.
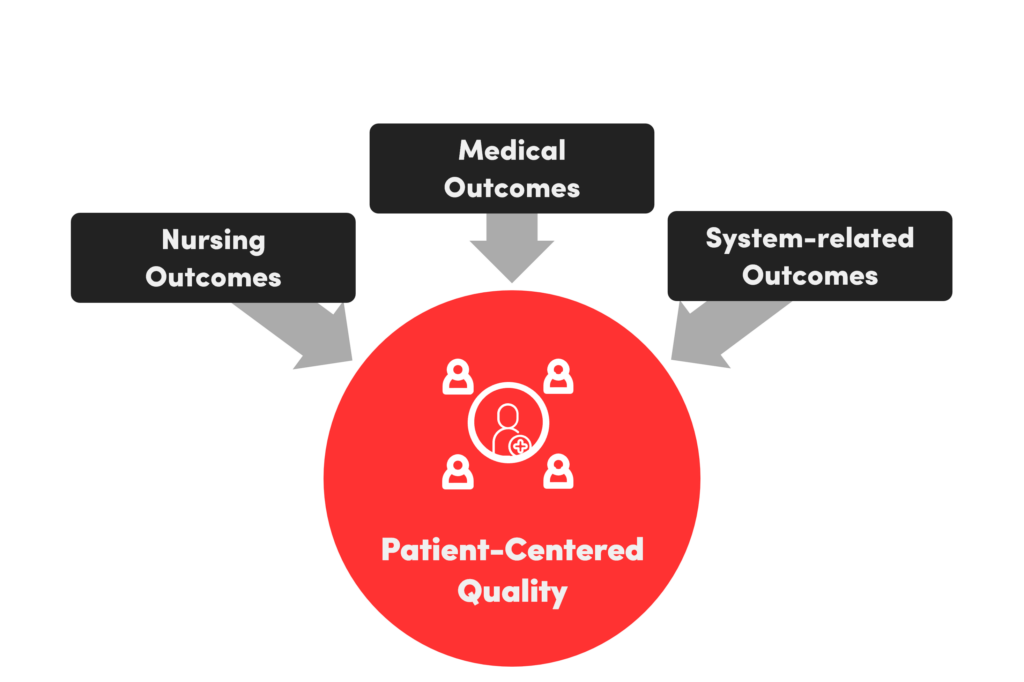
Transparency and employee participation form the prerequisite for a sustainable digital transformation as well as supported values. Value-based healthcare ensures patient and employee satisfaction. In the future, patient-centric service provision and self-determined work within a new error and feedback culture will play a more important role. In this Modern Workspace Guide against the background of the New Work movement, practical recommendations for action are presented using the example of personnel-intensive nursing services. In addition to the medical and systemic outcome, nursing care is essential for the recovery process. For the majority intrinsically motivated nursing staff, the nursing outcome is significant. To achieve this, we need to translate the care processes into a quality-oriented digital process thinking and combine utility and usability.
Index
Introduction
As value-oriented healthcare, in addition to the medical and systemic outcome measurement, the nursing outcome, which is significantly involved in the recovery process, is also of great importance for the majority of intrinsically motivated nursing staff. Therefore, we have to translate the care processes into quality-oriented digital process thinking and combine benefit and usability. Appeal as a nursing expert and health economist for system-relevant nursing:
- Digitization and change do not work alone. We must have the courage to cut back on old habits.
- Allow ambition for patient-centered service delivery as Value-Based Healthcare (VBHC).
- Less focused on efficiency, foundation of patient-centered and quality care.
- Feedback culture, creating space for participatory as well as patient-centered care processes.
- Interoperability, cross-sectoral interdisciplinary communication and digitally supported service delivery along the entire recovery process.
- Patient Reported Outcome Measures (PROMs) do not yet include specific PROMs on quality of care, capture correlation to staff satisfaction.
Method and sources: In addition to the positive effects of digital nursing applications (DiPAs) as administrative relief for nursing staff, there are other relief trends. For this purpose, our own 2021 survey with N = 51 in Swiss long-term care facilities forms as a major source of knowledge: Time saved by introduction of digital nursing documentation = 65 minutes calculated on one nurse per 8-hour shift. All data and information are based on exploratory surveys as well as cross-national literature research in the context of the 2022 defended doctoral thesis on digital maturity in nursing. The Swiss nursing initiative, with a concrete first implementation estimated for 2023, makes us rethink staff retention within the nursing profession. This resulted in the impetus for this Modern Workplace Guide.
Finding a solution: A high level of employee satisfaction based on evidence-based nursing services as well as nursing PROMs can significantly promote staff motivation. Nursing staff are characterized by high moral and ethical standards. Due to the current personnel situation in nursing, it is urgently necessary to introduce new workspace concepts and to push digitization as an administrative relief.
Lessons learned: A new error and feedback culture with personal responsibility must be anchored in the corporate culture in the future as a paradigm shift. Open and transparent communication and participation generate understanding through shared values. Understanding of the objectives in turn creates a sense of urgency. Above all, it is also about accepting digital change processes and being able to help shape them. As a basis for the well-being of patients, the culture of discussion must be promoted as an exchange between nurses and others involved in the service process. Initial cross-national, as well as internal, comparisons of reorientation emphasize the urgency.
For the commitment in the health care sector, especially for staff retention in nursing, the author was allowed to receive the international Outstanding Leadership Award health2.0 in December 2022 in Dubai.
1. Status quo of digitization and employee satisfaction
Digitization in Switzerland: The consistent introduction and use of mobile input devices with a uniform interface, non-proprietary applications for electronic patient files, billing, nursing diagnoses, medication administration, and intersectoral external access options for third parties involved in the treatment process are still largely lacking. Poorly readable fax medication orders and prescriptions continue to exist. Existing software solutions do not yet sufficiently map the time-intensive care aspect and evidence-based care planning processes. Communication is often done via email and with handwritten notes. Shared communication platforms are just being developed. The nursing discharge report and the hospital discharge documents are transmitted exclusively in printed form due to the lack of national strategies. Decision-making authority lies with the 26 cantonal health departments. The flow of information between the actors involved, the patients and their relatives, is currently concentrated mainly on personal conversations and telephone calls. For safe and effective medical and nursing care, no nursing PROMs, such as satisfaction with the exchange of information with the nurse, have yet been recorded. Education and agreement on data protection as well as the use of anonymized data for studies is hardly considered. In most cases, these are only rudimentarily included as an additional clause in the nursing home contract. Tablets with nursing applications for recording vital signs and documenting nursing measures are already being used in the non-inpatient area of long-term care. There are also fall sensors and applications, call systems, emergency alarms and, in isolated cases, wearables for measuring vital signs. Prevention and care during the accompaniment of chronically ill people are supported by telemedicine and early detection diagnostics with mobile applications.
Value-based healthcare and employee satisfaction: In a profession that is predominantly intrinsically motivated and characterized by high moral and ethical values, sustainable job satisfaction is essential for staying in the profession. This Modern Workspace Guide offers recommendations for action in this regard. Based on recorded nursing PROMs within a value-based feedback culture, further potential for employee satisfaction can be exploited in the future. This new research approach to quality of care in correlation with employee satisfaction needs to be exploratively expanded. A longitudinal study by the ZHAW Institute of Health Sciences as part of the Competence Network Health Workforce concludes: With better working conditions and career opportunities, nurses can be kept in the profession longer. Nine out of ten graduate nurses are willing to work in nursing under better working conditions in the next ten years. However, more than half of the 600 nurses surveyed said they often feel tired and overworked at work. About one-third said that a full-time position would be too physically and mentally demanding. According to René Schaffert, project manager of the aforementioned longitudinal study 2011 – 2019, the compatibility of family and career and having time for private life are the two most important points that need to be reflected above all in duty roster design. More regularity and consideration of individual duty roster wishes would be required. In reality, these expectations often cannot be met. This discrepancy correlates with job satisfaction and the thought of leaving the profession. With high intrinsic motivation and high quality demands, a discrepancy often arises between one’s own professional attitude and actual economic as well as resource-related conditions. Dissatisfaction and low-quality services can be the result.
The COVID-19 pandemic has shown that many hospitals are already working at the limit of their capacity. Less than one third of physicians and nurses in senior positions in Germany plan to continue in their current profession until retirement (M. Burkhart et al., PwC, 2022). According to a Swiss study “Stress in the Swiss workforce” by the State Secretariat for Economic Affairs, it is clear that 33 % from the education, health and social sectors have the feeling of being used up at work. In the social sector, the figure is 25%. One in five specialist nurses in the healthcare sector has already turned their back on the healthcare system after five years (SBK Pflegeinitiative, Ribi, Y., 2018). A shortage has long been warned about in Switzerland, but now there is a real lack of nursing staff. Hundreds of hospital beds are closed – and sick people have to wait. Three waves of infection are sweeping across the continent at the same time. One of them is particularly hard on children. Every month, 300 nurses in Switzerland leave the profession. The nursing crisis is escalating in Europe – and Switzerland is being hit hard. On December 15, 2022, around 100,000 nurses in the UK went on strike for 24 hours, the first time in the 100-year history of their union. The strikers cite low wages, mass exodus from the profession and the excessive demands resulting from the staff shortage as reasons. France complains of a regional exodus of nursing staff of 50% to the better paid Swiss border region (Bühler, S., & Wanner, A., ch media 22.12.2022).
2. Paradigm shift towards cost-benefit orientation
Value-added processes with proven patient benefits and good quality of life outcomes are to be expanded and simplified. The data on the best possible quality of treatment and care allow a basis for negotiation with the payers and a departure from the pure quantity principle with incentives for overuse and misuse. The quality of nursing care could thus help to determine prices. This is also the case in other industries (Barmettler, S., 2022). Following the Lean principle, wasteful processes without measurable patient-centered customer benefits are to be avoided. Employees are to be involved in process optimization through regular workshops (Krüger, R., et al. 2022). Redundancies should be questioned and eliminated. Patients should also be more involved in the provision of services in the future. The main aim is to assess how health status and quality of life measured in years (QALYs) improve over time. In the future, these should be able to flow into the payment system as key performance indices (KPIs) (Barmettler, S., 2022). The successful digitally supported service provision in turn serves as a basis within the feedback culture as well as a motivational basis for the healthcare staff. The Health Study 2022 (N = 2,136) of the Sotomo Research Institute shows that burnout sufferers clearly cite a lack of appreciation of their work as the number one cause of their illnesses (Hermann, M., et al. 2022).
3. Change in work culture
In the future, nursing staff will assume more responsibility and act in a more self-determined manner. As a result, the nursing profession will gain more creative co-determination and new competence profiles, for example in nursing IT, nursing controlling and nursing management. This makes the profession more attractive, independent of old hierarchical structures, and opens up new development opportunities with specialist areas. Digitization helps to reduce the administrative burden, so that more time can be spent on the actual people-to-people work.
A look at Germany: On November 20, 2022, at the congress in Berlin, the Handelsblatt Health Circle, together with Health Minister and epidemiologist Prof. Karl Lauterbach, posed the following question: How can our healthcare system, under the given circumstances, be consistently oriented toward patients/employees and value in the purpose of Value-Based Healthcare (VBHC)? Too little attention is paid to the process quality and sensitivities of patients. For us, creating a VALUE-BASED healthcare system means being oriented towards patient-relevant outcomes instead of proceeding with a “watering can” approach. The focus is on the patient’s quality of life with the correlation of resource-based time feasible as well as measurable quality of care. This allows us to actively guide the promotion of satisfied health professionals.
3.1 Reorientation of case numbers for value orientation
Currently, quality in the Swiss as well as in the majority of the European health care system is regulated by specifications on inputs and case number-driven Diagnosis Related Groups (DRG) processes, but too little by effective outcomes of treatments and care provision. The excellence would be to link the outcomes to the reimbursement system. The first pilot projects are already underway here. There is no way around the need for a radical cultural change in the healthcare system. Quality measurements at the hospital level, in the preclinic and at the employee level should be understood as an instrument for learning. The prerequisite for change is:
- Transparency and participation, an open culture of criticism and error are crucial.
- Standardize processes to a much greater extent and support them digitally. In this way, we can get by with fewer specialists and thus reduce the workload on staff.
- Because we standardize much more, we can align services more value-oriented and measure the outcome more easily.
Other industries, such as the airline industry, are further ahead. Safety first is the rule there, and that is the yardstick by which we are measured. Patient satisfaction should be given greater consideration in payer compensation and as a motivating factor for staff. If we can achieve this, we will have an incredible learning effect in the system, because everyone will then have the incentive to become better, and not the incentive to offer as much as possible with as few staff as possible (Handelszeitung, 2022).
3.2 Value-Based Healthcare as a New Meaning
Value-Based Healthcare (VBHC) means basing decisions about the delivery of treatments and the subsequent treatment pathway on the benefits to patients, rather than on financial targets in budgets and volume incentives in tariff systems. In this way, the daily work of health professionals becomes more “purposeful” again – the work makes sense again and fulfills one. It is about quality and patient benefit and no longer just about the money. A positive effect on job satisfaction can be expected (Liberatore, F., 2022). Measuring performance and patient satisfaction are key factors in ensuring the quality of value-based medical services and care. In the health care system, there are currently efforts to make medical and nursing services more transparent, not only for the health authorities and payers. Medical and nursing services are to take better account of success in evidence-based care in all care-providing organizations. Patient-Reported Outcome Measures (PROMs) form the basis for this. They capture a person’s perception of their own health through questionnaires. They allow patients:inside to report on their quality of life, daily functioning, symptoms, and other aspects of their health and well-being. The reference point for attributing meaning is the experiencing care recipients themselves. Decision-making criteria in care should be based on scientific evidence and expertise, care receiver experience, and caregiver responsibility with available resources. Patient satisfaction includes factors such as how the treatment and nursing care was and whether patients:inside had the opportunity to ask questions of the nursing staff. Relevant factors from the patient:s perspective are the burden of limitations and discomfort in daily life. As a cross-sectoral transition, the transition to aftercare is perceived as an important interface for everyday life.
Example Switzerland: According to the Bertelsmann Foundation “PROM an international comparison”, there is still no national Swiss strategy in this regard (Steinbeck, V., et al., 2021). Binding regulations exist so far only at the cantonal level. But what does this have to do with New Work in the context of a digitalized nursing Nursing4.0? These and other questions of employee satisfaction and staff retention are discussed below as a Modern Workspace Guide.
3.3 Holocracy in nursing – does it work?
First of all, a successful example from outpatient nursing practice which, as a holocratic management model, sees the quality of nursing care as the basis for employee satisfaction. The nursing staff is characterized by high quality standards and values in which the quality of their own actions is paramount. The charismatic Dutchman Jos de Blok, who was awarded the Albert Medal, founded the community-based and customer-oriented non-profit organization “Buurtzorg” in 2006 with a team of four nursing professionals and has thus largely revolutionized home nursing, or rather reduced it to what is really important: people. He has succeeded in reducing the administrative burden on the nursing staff, while improving the quality of care and thereby increasing the job satisfaction of the employees. Everything derives from this vision, because values get their radiance when they are lived.
Concrete successes: no managers:inside, an innovative IT system and 40% lower costs as a competitive advantage. The development showed, from a team with four employees – to today more than 1’000 teams with 14’000 employees in only 12 years. In addition to the Netherlands, the system is used in 26 countries (USA, Sweden, UK, Japan and China). Successfully, 30% less nursing effort was realized. Costs per patient were almost halved and job satisfaction doubled at the same time (FutureHealth, NZZ 2022). In Switzerland, there are already Spitex organizations (Spitex = companies for outpatient care), which orient themselves on the Buurtzorg model and do so successfully. The goal of care is to spend 40 hours less per patient per year and to focus on the needs of the patients instead of money (Future Health NZZ, 11.2022). Change Management: A change of a rigid system is only possible if one can understand the reason and the sense of the change.
4. Humanity over bureaucracy – managing quality
Quality indicators and PROMs in nursing should be used as a basis for planning and controlling nursing measures. Feedback on successfully performed care services (measurable performance success, satisfaction and quality of life) as mentioned above in the Buurtzorg model in the holocratic approach of self-control for long-term care, promotes self-control as well as staff motivation. In order to be able to implement continuous and efficient self-controlling, it should be possible to derive nursing outcome quality from routine nursing documentation in the context of a secondary data analysis. Nursing outcome quality supplemented by satisfaction is understood as the degree of congruence between outcome and nursing goal (Korečić, J., 2003). Therefore, nursing outcome quality can be defined as measurable changes in professionally assessed health status, quality of life, and satisfaction of those affected, as well as the result of framework conditions and measures of nursing care (Liu, Y., et al., 2014). The PROM measurement domains differ as follows for this purpose:
In addition to length of stay, fall/decubitus rates, recording of redundancies, turnaround times, medication errors, postoperative infection rates, this includes above all the patient-oriented measurement of the mentioned quality factors as well as the quality perception of the nursing recipients. Objective of data collection: to investigate the timing of PROM collection and the impact on bias in QALY estimation for the economic assessment of Quality-Adjusted Life Years (QALYs). Resulting Potential Improvements:
- Lean medical, nursing and administrative processes
- Quality assurance
- Performance orientation and feedback culture
- Capacity planning and control
- Digitalization and automation.
5. Potential for relieving the burden on personnel
The shortage of healthcare professionals is the dominant issue in the healthcare sector. The shortage is now so severe that long-standing demands of professional associations, such as that of the Swiss Professional Nursing Association SBK-ASI for better working conditions and higher wages, are being implemented with employee-oriented rostering. In addition to the creation of the digital prerequisite as a relief in the daily care, the fact of the staff shortage, further development of the nursing profession with increasing documentation costs to payers. With simple speech recognition tools, nursing could be supported in their daily work processes and documentation of the nursing process. Speech recognition is currently not yet mature or useful in all areas of nursing documentation. In order to achieve a successful use of speech recognition, it would be necessary to survey target and usage scenarios as part of a project. It is important to define which activities are to be documented with speech recognition in the future and how the documentation is carried out in relation to the current status (Redl, V., 2022).
In order to record the digital maturity level and the current state, the PDS maturity model in nursing care, which was created specifically for this purpose, is helpful. At the end of 2021, the average maturity level in long-term care facilities in eastern Switzerland was 88.2 points, a total of 5.4 from maturity level 1 to 8. The next highest level, 6, is associated with the consistent introduction of mobile devices. This maturity level starts at > 90 points. No institution has yet been able to achieve maturity level 8 of “Excellence” with > 120 points in any discipline. The main functions ‘master sheet’ and ‘wound documentation’ as an integrative component of the entire digital patient documentation scored particularly positively in maturity level 7, which has already been achieved. In order to make positive changes and existing systems assessable, it is necessary to have a practicable tool available for self-evaluation in nursing. The use of a digital form of documentation has an impact on the way in which information relevant to nursing and quality can be recorded, processed and used. In the context of the digital transformation Nursing 4.0, digital nursing documentation will play a significant role in future cost savings, staff reduction and quality assurance. Even before the digitization of nursing documentation, the administrative effort in an 8-hour shift averaged 47% at 3.8 hours. After digitization, the administrative effort averaged 33.5 %. Thus, for every eight employees, one full-time position could be saved for the actual person-to-person activities and the workload could be significantly reduced as a result (own survey 2021, Switzerland N = 51).
6. New Work in Nursing
The term was coined as early as the 1970s: In his philosophical work, Frithjof Bergmann came to the conclusion that the work people really want is characterized above all by freedom, independence and participation – and that to a high degree. In the meantime, however, the term “new work” has come to be understood even more broadly, as it simultaneously describes structural and technological changes in the world of work – and thus also social change. New Work and resilience in care are becoming increasingly important for staff tied to the company. In 2021, Germany, as a European reference example, counted 4.6 million people in need of care in outpatient and inpatient care – and the trend is rising in view of demographic change. Germany already has a shortage of around 376,000 care workers (Federal Employment Agency, 2022). Looking at Switzerland: there, more than 13,000 nurses are currently being sought with advertised vacancies. Nurses are system-relevant carriers of the health care system. In nursing, they work and make decisions autonomously. In the future, nurses will be significantly involved in all decisions in the health care system. The shortage of qualified nursing staff will be reduced by measures in education and working conditions (SBK-ASI, 2021).
However, the image of nursing has changed for the worse in the last 10 years. Nurses are confronted with economic issues and increasingly have to reconcile professional ethics with economic goals. Nursing services must be processed, and that as efficiently as possible due to the lack of time and personnel. The economically oriented management and the increased workload make the nursing profession unattractive. What is lacking are not only resources, but above all opportunities for employees to participate in shaping their own work. This is precisely where the New Workspace concept comes in: it offers more opportunities for development, but also more responsibility, making the job description and career in nursing much more varied and promising. In addition to the quality philosophy, the following approach also prioritizes lean (relieving) as well as value-creating process orientation.
Lean and Kaizen: in addition to digital documentation of patient care, the demand-oriented design of telemedical consultations and cross-sectoral lean care processes offer great potential for improving quality and reducing workload. The concept of the Advance Practical Nurse (APN) can counteract the increasing shortage of general practitioners in rural areas. As an outpatient and integrative approach to care, APN activities can relieve the burden on the local clientele. Activities are taken over which were previously considered to be predominantly medical activities. This also means a responsible upgrading of the nursing profession with further specialization options, for example in diabetology, palliative care, wound management or postoperative follow-up care. Projects to this end are already underway at the Hirslanden Group in Zurich and the Zurich University of Applied Sciences (ZHAW). The shortage of skilled workers makes it clear that we need to rethink our approach, especially in long-term care, in order to attract junior staff and retain qualified personnel. This is precisely why it is important that we reflect on existing work structures in order to create an attractive workplace with prospects. Away from flexible working hours, New Work holds promising measures to realign working conditions with the needs of caregivers and create space for the development of potential (Bundesagentur für Arbeit, 2022).
6.1 Implementation of New Work
New Work: What is New Work anyway? By definition, New Work is “an approach and a movement at the same time. The goal is a change in the understanding and design of work in practice.” Economically oriented management, staff shortages and increased workloads are making the nursing profession unattractive. At the same time, little or nothing is happening in terms of further development of the nursing image – many work structures are rigid and long outdated, and there is a lack of perspective for the future of nursing. This causes frustration and listlessness among nursing staff (Hackl, B., et al., 2017). The concept of New Work offers solutions for exactly this. More opportunities for co-design and development, but also more responsibility arise, which make the job profile and career in nursing much more varied and promising. While the classic concept of work is characterized by hierarchically organized structures and rigid processes, the New Work approach asks us new questions (Dovgucic, A. 2022):
- How do I have to shape my work so that it fulfills me?
- How would I like to work in the future and contribute in a self-determined way?
- What is the individual potential of each person?
6.2 New Workspace – 6 Requirements
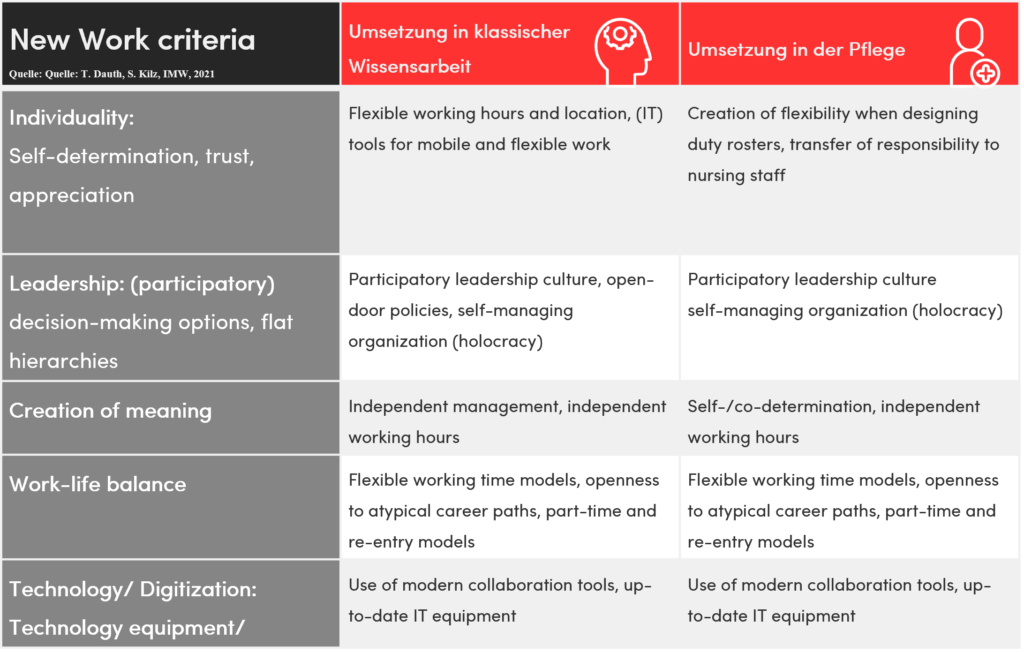
New Work requirements can be divided into six areas of daily work:
- Individuality
- Leadership
- Sense of purpose
- Flexibility and compensation
- Feedback culture
- Technology and digitalization (Dauth & Kilz, 2022)
New Work in Nursing – Ultimately, nursing resembles traditional knowledge work in this regard – as elaborated on the basis of the six New Work domains (Gentner, S., 2022).
1. Individuality
This is about self-determination, appreciation and trust – knowledge work is based on flexible working, i.e. time- and location-dependent, which make the use of relevant tools useful. Similarly, nursing can proceed by making duty rosters more flexible with an intelligent shift planner and by handing over responsibility to the nursing staff.
2. Leadership
New Work also means involving staff in decisions and keeping hierarchies as flat as possible. In both knowledge and care work, “open door” policies and self-managing organizations can be implemented.
3. Sense-making
With regard to traditional knowledge work, this primarily means self-responsibility – both in terms of leadership and working hours. For nursing, self-determination and autonomous working hours could be meaningfully brought to life with the agreement of trust-based working hours and intelligent time recording. As a motivational basis, nursing PROMs are also a relevant factor in creating meaning.
4. Flexibility and compensation (work-life balance/ blended)
In traditional knowledge work, this criterion can be mapped with flexible working time models such as flexitime, part-time and return-to-work models, but also openness to atypical career paths and remuneration – and care institutions are also able to do this.
5. Feedback culture
Open cooperation based on respect and trust is supported by constructive feedback. It is equally important not only to create physical and temporal space for the development and testing of ideas, but also to live a goal-oriented tolerance of error for self-determined work. In particular, care recipient satisfaction should be measured and openly communicated as PROMs. These serve as a basis for motivation as well as job satisfaction, and thus in turn in the medium and long term also for psychological resilience and prevention of leaving the profession. The companies can thus position themselves well and actively manage their image for recruitment.
6. Technology and digitalization
If traditional knowledge work relies on the use of modern tools for collaboration and administrative relief of a modern IT infrastructure, this is equally true for work in the care sector.
7. New Working Guide Recommendations for action
Recommendations for action for leadership and personnel management can be derived to counteract the shortage of skilled workers by upgrading the work in nursing. Above all, the empowerment and recruitment of staff are also important.
7.1 Feedback culture
A change to a feedback culture in the working world must be supported by the entire company and the clinics – the management plays the decisive role here: it needs the necessary know-how to be able to master the challenges and effectively exploit the enormous potential. It is essential not only to inform staff comprehensively, but also to involve them intensively. Zero tolerance for errors characterizes the profession and is justified for patients, but not for the employees themselves.
Staff discussions: In nursing, motivation and plannable workload peaks are in demand. Managers should therefore regularly find out what requirements the current working conditions entail – and how these can be optimized.
7.2 Quality analysis and working conditions
Important insights can be gained from the analysis of a typical workday, such as work peaks that can lead to the revision of shift schedules or working hours. In this way, a more flexible approach to the respective needs can be realized (Gentner, 2022). And that is precisely the point: New Work focuses on a high level of work motivation. This is ensured by various factors, including good working conditions, remuneration, a good relationship with the manager, and a fair corporate culture. Nurses have chosen their profession primarily for personal fulfillment. They want to help people, to create a purpose. It is therefore essential to organize the work structures within a care facility in such a way that fulfilling and attractive work becomes the focus again. This also includes the explained measurability of care quality from the perspective of care recipients to successfully implemented care measures. For an engaged design of nursing tasks in the purpose of New Work, there needs to be freedom for nurses to contribute with proposals for action and to be creative (Frauenhofer Institut, IMW 2022). In this context, the nursing management has the task of creating a trusting and inspiring working environment. This includes: lots of open communication. Involving the nursing staff in decision-making processes creates transparency and acceptance. Giving freedom of action and personal responsibility offers the opportunity to help shape work processes (Hackl, B., et al., 2017). The basis for this is appreciation of the nursing staff through trust, a new working style with personal responsibility, and flat hierarchies (Bovenschulte M., et al., 2021).
Successful Swiss examples of self-organization in acute care are the hospital of the University of Basel and the Lucerne Cantonal Hospital. According to the nursing director of the Luzerner Kantonsspital Mr. Döring-Wermelinger in the panel discussion at the IFAS Expo on 26.10.22 in Zurich, the wage costs could be reduced significantly. In a patient-centered and value-oriented health care there are mainly positive effects on:
- Efficiency of operational processes and decision-making.
- Satisfaction of employees and care recipients.
- Better self-control/self-responsibility, according to the Dutch Buurtzorg model.
- Better group cohesion as a basis for agile adaptability to new challenges.
7.3 New competence profile requires knowledge enhancement
The tasks that nursing staff have to perform are wide-ranging. They include: general nursing care tasks, medical assistance tasks, logistical and technical tasks, transport and cleaning tasks, and documentation and administrative tasks. The competence profile is now expanding to include self-responsibility, media and digital competence. This implies the following core message: digital processes can only be as good as the staff is empowered and able to control them. Bad processes – remain digitally bad processes. The willingness of healthcare staff to change is 2.6, below the median (0 = willing to change; 6 = resistant to change) n = 512 (Angerer, A., 2012). This is also consistent with recent surveys. Results from 2022 point to efficiency as a motive for using known digital technologies. The willingness of nursing staff to use digital technologies is generally high. Management measures can provide a structural framework and training so that nursing leaders can ensure their staff’s commitment to using even unfamiliar devices (Korte, L., & Bohnet-Joschko, S., 2022).
7.4 Leader functions and new requirements of co-creation
Leaders are taking on new functions and roles.
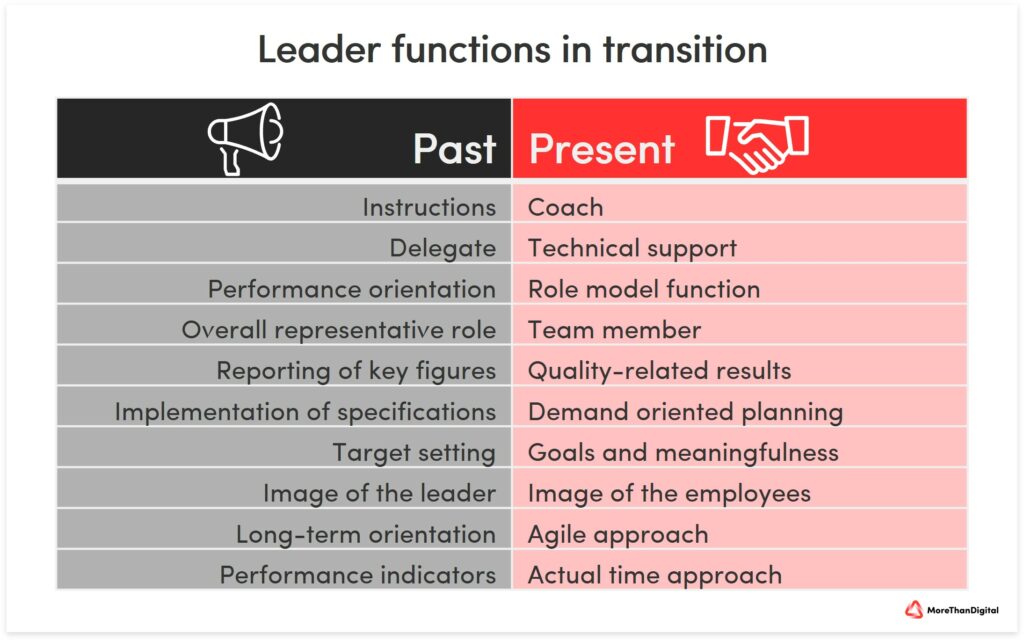
It has proven effective to communicate smaller milestones with a short-term planning horizon as fulfilled and thus to keep the motivation of the employees constant. But employees are also allowed to undergo a profound change in the previously strongly hierarchical hospital structures. They have to take on new responsibilities and work towards the overall goal.
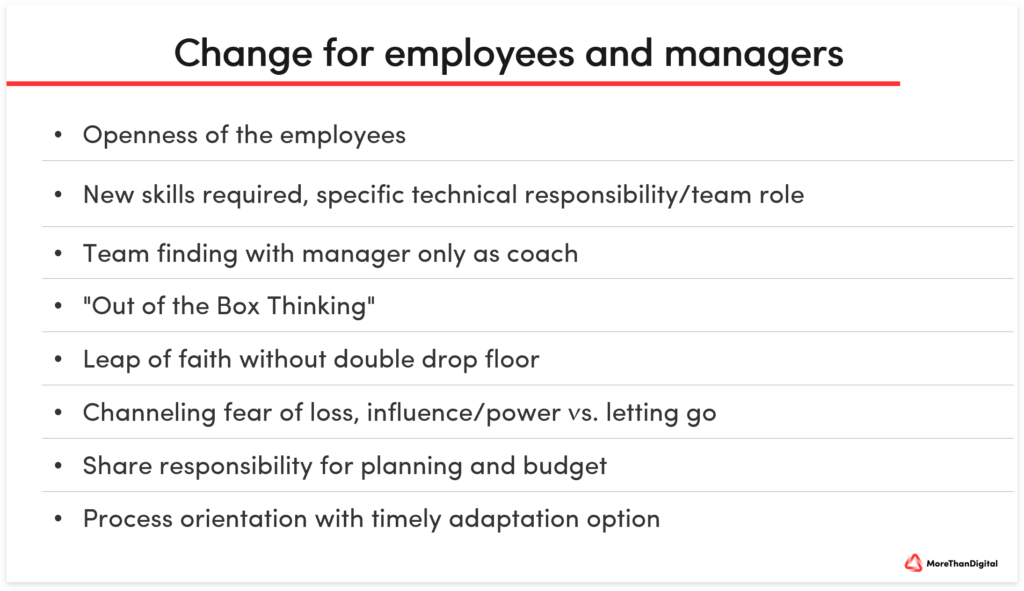
Flat hierarchies and interdisciplinary cooperation at eye level help to shorten official channels and enable direct (interdisciplinary) exchange between employees and colleagues from other departments. Questions can be clarified more quickly, and the focus is on more flexible work that is tailored to the needs of the clientele. Feedback discussions, in which nursing management and nursing staff openly exchange ideas, together with mutual trust and the possibility of individual further training opportunities, form the basis for an attractive working environment in which appreciation is lived (Dovgucic, A., 2022). The term co-creation is often used. This describes an approach to work that enables employees to develop solutions independently in the team – without the stipulation or influence of a nursing management. The manager takes a back seat in the self-organization process. They merely create the framework conditions for self-determined and pleasant work. Partially autonomous teams, for example within the individual shifts, organize themselves and the daily nursing tasks themselves. The result is greater satisfaction, more influence and more success at work (Bovenschulte M., et al. 2021).
7.5 Retaining staff and attracting employees
With the Corona crisis as an accelerator, new work models are now rapidly gaining acceptance. The crisis-induced surge in digitization is promoting new work structures characterized by work-life blending (more spatially and temporally self-determined work), collaboration and remote work. Corporate cultures are becoming more agile and adaptive, while employees see themselves more as problem solvers for societal future tasks (Mahlodji, A., 2021). The systemic relevance of nursing is undisputed in this context. Especially with regard to the COVID-19 pandemic and the resulting high turnover rates, this has been clearly demonstrated (Dauth & Kilz, 2022). Factors such as meaningfulness, design opportunities and work-life balance have become more important than purely monetary factors. A new view of the significance and purpose of doing business is emerging. The younger generations in particular, Generation Y and Generation Z, are aware that the promise of eternal economic growth, which has provided meaning in life up to now, cannot be fulfilled if the basis of life for everyone – the planet Earth and its resources – is ruined in the process (ZukunftsInstitut, 2022). Corporate culture, sustainability and corporate social responsibility of a company form the basis for the corporate image, which have become more important in terms of meaningfulness. In addition to the advantage of being able to position itself well as a responsible company and thus become attractive for employees in the competitive market for skilled workers, such a reputation also increases the satisfaction of the clientele and thus the resilience of the company.
Effectively implemented care technologies and New Work strengthen the resilience of care teams. Important factors of resilience are appreciation and transparency, consequently the feeling of time feasibility, a positive basic attitude and safety aspects. The services provided and successes achieved, as described earlier on outcomes and value-based healthcare of PROMs, need to be made visible and communicated to staff. The perspective of care recipients has often been missing.
Solution approach: show the contribution to the whole and celebrate successes such as care figures, positive customer feedback and successful care interventions together. Some Swiss companies are currently only reactively trying to counteract the nursing staff shortage with more pay or 80 percent working hours with full pay. The Aarau Cantonal Hospital wants to be able to recruit nursing specialists better in the future with a recruitment office in Rome. Mr. Fabio Blasi, head of personnel recruitment, is leading this future project (Jonsdottir, E., 2022). These unfortunately only reactive measures, as well as the WHO recruitment codex for richer countries, will not be discussed in detail here. Of course, everyone wants “more money”, but belonging, social identity in the company and appreciation have become more important to retain staff in the long term and to be able to attract new qualified employees. However, there are managers who are basically convinced that an unexpected team pizza is more motivating than money (Tschudy, D., 2022).
Not only the topic of working hours, but also the place of work is undergoing radical change. The Corona pandemic has shown that remote work is an important component of New Work – and it works (Mahlodji, A., 2021). During the pandemic, telemedicine nurses were able to work remotely, without real contact with patients, to relieve the burden on the healthcare system. One example is Medi24 Service AG in Switzerland. Temporary assignments: in the rapidly developing gig economy, the growing labor market of freelancers and temporary agents in the care sector, work is increasingly linked to the need for weekends off and scheduled shift work. The permanent staff, however, is confronted with a proliferation of administrative tasks, which causes dissatisfaction in several respects and thus a loss of image for the industry. Key influencing factors in the gig economy are:
- Flexible working models – shift work including weekends and holidays as well as on-call duties.
- Compatibility of family and career.
- Comparatively better pay for temporary employees compared to permanent staff.
- Services of permanent staff hardly appreciated.
- Work tasks and time continue to increase.
- Rigid hierarchies and outdated management style.
- Hardly any development opportunities.
- Threat of overload – physical, emotional and psychological.
Important: It is therefore urgently necessary to make the profession more attractive in order to avoid a complete drift into the gig economy. The levers for companies have been described above.
8. Future challenges
According to the Swiss Nursing Association SBK-ASI and other official sources, Switzerland will have a shortage of up to 65,000 nurses in inpatient and outpatient care in 2030. The principles of the World Health Organization (WHO) include a recruitment code of conduct. This prohibits recruitment practices of healthcare personnel from richer countries abroad. The most important goal is for countries to train their own health workers. The shortage of nurses is a global problem. According to estimates, there will be a shortage of 18 million nurses by 2030 to achieve the Sustainable Development Goals, writes the Federal Office of Public Health FOPH (Bühler, S., & Wanner, A., ch media Dec. 22, 2022). Germany has a shortage of 517,000 healthcare workers, according to data from the Federal Ministry of Health and federal and state statistical offices. An increase in the need for nursing care can be assumed. Looking at Germany: in view of the shortage of skilled workers, the German Professional Association for Nursing Professions (DBfK) has warned of the collapse of the system. To avoid this collapse of the system in the medium term, there is currently a shortage of 200,000 full-time employees, according to the association. At the same time, the number of respiratory illnesses is rising across Germany right now. “Up to 70 percent” of nursing professionals work part-time. Sickness rates are increasing because of the high workload, as well as work compression due to the staff shortage (BR24 Editorial, 2022). Especially in hospitals, “safe and high-quality care is hardly possible anymore,” said the DBfK chairwoman. The shortage of nursing staff recently became particularly apparent in children’s hospitals, where some beds cannot be operated due to a lack of nursing staff, according to the German Interdisciplinary Association for Intensive and Emergency Medicine (BR24 Editorial, 2022). Against this background, it seems essential to address the questions about the “working world of nursing” as follows.
- What demands do the new generations of caregivers and already experienced caregivers have on their employers?
- What is the relief potential of new technologies such as artificial intelligence or robotics to digitally map and support manual processes and tasks?
- How can we meet the growing demands and better-informed patients for more service, comfort and rapid support from staff?
The focus of these considerations should always be on the employee and his or her needs in terms of work tasks and environment. Because especially in personal services such as nursing, “healthy and satisfied employees are the elementary prerequisite for needs-based, high-quality and economical patient care”. The focus on individual care and attention for each patient without time pressure as well as the pursuit of purely economic interests is in the foreground for many nursing staff (Dauth, T., & Kilz, S., 2022). Not only the voting success of the Swiss nursing initiative on 28.11.2021 under initiation and cooperation of the Swiss Nursing Association SBK-ASI with the International Council of Nurses ICN has given the impulse for change in nursing. Companies in Switzerland are forced not to wait for the policy to be implemented. Some hospitals have reduced weekly working hours by up to 20% for the same salary with campaigns such as “Strong together – against the shortage of skilled workers”.
The world of work is undergoing fundamental, technology-driven and social change. This is creating new challenges for companies to position themselves as attractive employers. New Work with self-organization and a new value orientation is seen as the answer to the current (and future) shortage of skilled workers in the care sector. In addition to the low wage structure, the inadequate compatibility of work and family in shift, on-call and weekend service are the main reasons for not remaining in the profession. But also the already explained low appreciation and rigid hierarchical management with a lack of development prospects make nurses consider changing the profession. Not to mention the increasing compression of working hours and tasks with the risk of physical, psychological and emotional overload (Dauth & Kilz, 2022). As previously explained, the aforementioned characteristics lead to the declining attractiveness of this profession and, as a result, to recruitment problems with high sickness rates and fluctuation. The intrinsic factors of appreciation, co-decision-making, work content and personal development opportunities are particularly important for long-term motivation.
8.1 Drivers of change
As drivers of change, there are two dimensions, the societal level and the corporate level.
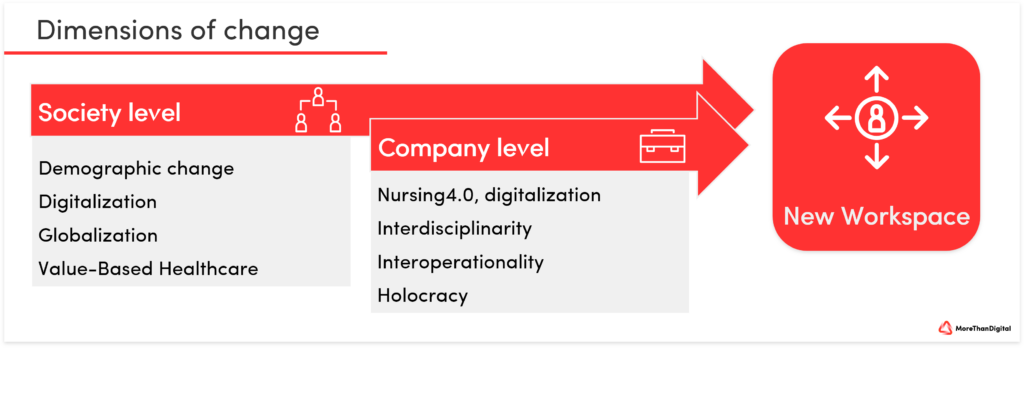
In addition to the patient-centered performance orientation, the work as a self-directing collaborative and transparent performance fulfillment comes to the fore. See also: Retention Management Healthcare. Work is seen as an opportunity for self-actualization with higher purpose. Only 28.4 percent of nurses agree with the statement that they can help people in the occupational field. For nurses, who have chosen the profession with a high intrinsic motivation and mostly out of conviction, this is obviously no longer true (M. Burkhart et al. PwC, 2022). A lack of recognition in nursing is also reflected in the fact that nursing activities are not relevant, or only to a subordinate extent, in billing.
8.2 New Work Criteria
In nursing, the actual person-to-person activity remains central.
Through the illustrated criteria, the prerequisite for autonomous and self-determined work can be created. The manager should be able to deploy and promote employees according to their potential and competencies, to relinquish control and power, and to delegate responsibility. This can increase job satisfaction, as employees are thus able to achieve their goals and pursue meaningful tasks (Dauth, T., & Kilz, S., 2022). In this context, new work in nursing is understood as a comprehensive transformation of work delivery, work practices, work organization, and corporate management with the advent of digitalization (Hofmann, J., & Günther, J., 2019). The transformation is taking place at both the societal and the corporate level. Associated with this are the new requirements and competencies described for managers and employees (Dauth, T., & Kilz, S., 2022). This is the only way to create the conditions for autonomous and self-determined work. Holocracy approach: employees write needs-based rosters, versus institutions determine the needs. Open communication and a good feedback culture enable a “we-feeling” and a less disruptive approach.
8.3 Work-Life-Blending versus Work-Life-Balance
The eternal search for a balance between work and free time is always fraught with conflict, especially in nursing shift work, because something always comes up short. Work-life blending and participative duty scheduling equalize these conflicts. Where the boundary between work and private life disappears, personal needs can be better taken into account during the course of the day. This not only creates relaxation and a better quality of life, but also increases the enjoyment of work. Improving the work-life balance and caring for family members is a key need for caregivers. This requirement could be met by introducing innovative working time models. Examples include models such as job rotation or job sharing. The latter in particular offers numerous advantages. Job sharing creates synergy effects, as two people contribute and share their knowledge. In addition to these working time models, time corridors with flexible start and end times of duty (taking into account staffing peaks) and shortened duties can also be an attractive option for caregivers, especially parents. Another option is so-called long-term accounts, in which working time can be saved for phases of life in which one cannot work full time, e.g., during a family phase or when caring for relatives (Dauth, T., & Kilz, S., 2022). The company health management BGM (stress management), supervision and a regular exchange form the basis for the well-being and performance.
8.3.1 Future viability through resilience instead of efficiency
What is needed are not even more sophisticated reporting structures or an even clearer management cockpit, but rather a confident and meaningful way of thinking and acting when dealing with nurses and patients. Only when the permanent rationalization and purely monetary output optimization of all processes is no longer a priority does room for further development arise – for leeway that makes companies more agile and resilient. In the future, automation and artificial intelligence (AI) will primarily replace repetitive and uncreative jobs that were not very fulfilling for humans anyway. Empathy, intuition and creativity, on the other hand, are qualities that cannot be replaced by machines – and are essential for the future of successful companies (ZukunftsInstitut, 2022).
8.3.2 The 30-hour week as the new full-time
The economist John Maynard Keynes predicted the 15-hour week as early as 1930. What will happen next? Will Keynes’ prediction come true after all? After all, there are still 8 years to go until 2030 and technological change is advancing faster than ever (Ohanian, M., 2016). In terms of working hours, Scandinavian countries are already living the working ideal of the future. Less is more. Working time is no longer understood as a weekly continuum, but as a flexible contingent that can be adapted to individual situations and life phases. The 30-hour week as full-time sometimes makes people more productive and reduces sick leave (ZukunftsInstitut, 2022).
8.4 Importance of digitization
Digitization and new technologies are bringing caregiver time back into focus as a person-to-person activity. Work processes that used to involve a lot of effort now take just a few clicks thanks to digital innovations. Collaboration across locations is no longer a problem, and knowledge sharing and networking are becoming increasingly important. In care, new technologies and digital care applications are helping to relieve administrative workloads and improve the quality of care. By helping to mobilize and care for people in need of care, and by supporting therapeutic measures and automatically transferring them to the care documentation, intelligent solutions create more time for nursing care. This makes work easier and makes the job more enjoyable. In the end, both caregivers and nursing recipients – regardless of shift, department, and outpatient or inpatient facility – benefit from a relieved, decelerated, and fulfilling work environment. New companies such as Lindera with a mobile application for fall prevention and risk assessment, convey more safety with less fear of falls (Dovgucic, A., 2022). Mobile documentation integrates documenting into the care process, reduces workflow interruptions, saves time and secures information (Lizarazo López, M., Tiryaki, S., 2021). This allows for significant time savings, see also: Maturity Assessment of Swiss Nursing Facilities 2021. This prevents sources of error, duplicate documentation structures with pen and paper as well as redundancies on the computer, loss of information and brings the documentation activity closer to the care recipients. In order for these relief effects to be felt in the work process, digital documentation using mobile devices is essential (Lizarazo López, M., Tiryaki, S., 2021). If the documentation and administration work that is a nuisance for many caregivers is automated with the help of intelligent tools, there will be more time for the important work on and with those in need of care.
There are already numerous intelligent tools that effectively support companies of all sizes. In addition, sensor systems, along with communication robots, tablets and call systems, help relieve the physical burden on nursing staff as fall prevention, since fewer falls also reduce the frequency of heavy lifting. In addition, the data aggregated in the digital documentation system helps improve care quality and patient safety. These are said to help PROMs provide a more holistic view of care recipients, better monitoring of nursing interventions, and easier adherence to guidelines and nursing goals. The increase in the sense of safety perceived by a large proportion of the nurses surveyed has a positive impact on their job satisfaction. The avoidance of errors, effective prevention measures, reduced walking distances, faster documentation and simpler communication also result in gains in effectiveness and efficiency. Typically, time savings are used to spend more time with care recipients, which also increases caregiver satisfaction. (Lizarazo López, M., Tiryaki S., 2021).
8.5 Employer Branding
The implementation of New Work opens up completely new questions that companies must address together with their employees (Dauth, T., & Kilz, S., 2022). For example, do labor laws – the guardrails within which companies operate – still reflect the reality with regard to New Work? Do established notions of working time legislation and rostering need to be reconsidered? How can the self-responsibility of employees in companies be reconciled with the traditional ideas of “employers” and “employees”? And what new demands do flexible forms of work place on the occupational safety and recreation of employees? Participation, transparency and freedom of decision are prerequisites for retaining nurses and attracting new nurses. The logic has thus been reversed: employers themselves must become applicants among the workforce (So called – employer branding). Personnel development, further training and career opportunities are also a prerequisite for remaining attractive as an employer.
9. Core message of Value-Based Healthcare
VBHC means basing decisions about the delivery of care and the subsequent treatment pathway on the benefits to patients rather than on financial targets in budgets and volume incentives in tariff systems. In this way, the daily work of health professionals regains more “purpose” – the work makes sense again and fulfills one (Liberatore, F., 2022). It is about quality and patient benefit and no longer just about the money. A positive effect on job satisfaction can be expected in the medium term.
10. Lean management creates innovation potential
The aforementioned practical examples in acute care at the University Hospital Basel and the Cantonal Hospital Lucerne prove that measures for knowledge and competence building also promote job satisfaction and the innovation potential of employees. However, structures for knowledge management and knowledge generation are predominantly hardly present in outpatient and inpatient long-term care facilities (Dauth, T., & Kilz, S., 2022). The following enablers for an innovative environment are oriented according to the Japanese Gemba philosophy as part of Kaizen (Kanban) and Lean Management. In the purpose of continuous improvement, it is important to know the enablers well in the context of an actual state.
Gemba – 現場, or Genba, means “the actual place” in Japanese. Lean practitioners use gemba walks to drive strategic goals. Unlike typical Western management models, where managers stay away from employees in their “ivory offices,” Lean encourages going on-site (to Gemba) to observe, learn, connect with teams, and offer help. The goal is to find out what is actually happening in the workplace and in the workflow.
Step 1: Tell the team ahead of time what you will be doing!
Step 2: Be prepared. It is a good idea to have a plan and know what aspects and questions to ask the team are important.
Step 3: Go to where the work is being done and observe it with them in the emergency department, for example. It is critical to go to the real place where the work is being done and observe.
Step 4: Respect your employees, don’t judge. It is important not to judge or supervise employees. The Gemba Walk should give you further insight into what you have already seen on your Kanban board (tool for planning and control).
Step 5: Unlock knowledge work and improvement opportunities. In addition to the insights gained about the service process, caregiver concerns, participation levels, digital (technical) support and work intensity also offer important insights. After an assessment of the current situation of the core process and the administrative processes, measures and the time frame for a New Work concept can be derived, and the corresponding employee-focused redesign can be implemented with further milestones.
11. Framework conditions for sustainable job satisfaction
A change in thinking has begun and the following framework conditions represent the basic prerequisite.
- Opportunity-oriented “digital mindset,” open error culture.
- And a high degree of adaptability in organizational and work processes.
- Monitoring the effects of technologies on interaction with caregivers.
- Mobile documentation/voice input, consolidation of nursing-relevant information at the “point of care”.
- Use of freed-up time resources to relieve the burden on caregivers and improve the quality of care.
- Information flow across structural, sectoral, institutional and hierarchical boundaries.
- Greater promotion of regional and supraregional cooperation.
- Networking to create places of support, knowledge sharing and reflection.
- Creation of low-threshold innovation support geared to the specific needs of care institutions in order to do justice to different levels of development and prerequisites in care practice.
- Ensure permanent funding within the framework of regular structures, to perpetuate transformative technology-based care settings and enable rollout (Lizarazo López, M., Tiryaki, S., 2021).
- Change management: create positive encounters (short-term milestones) and positive emotions.
Four positive interactions are essential. Communicate purpose, meaning, successes, and goals transparently.
Technical support: telemonitoring systems for monitoring vital signs and the supporting hospital information system (HIS), the electronic patient record/dossier (ePA/ EPD) or the use of robots. The use of these technologies is associated with the hope of improving the quality of care, facilitating documentation, saving time as well as thereby having more time for direct care of those in need of help and being relieved of routine tasks as well as physically heavy tasks (Dauth, T., & Kilz, S., 2022).
Otherwise, the shortage of skilled workers in this sector will continue to worsen in the coming years due to demographic change and the increasing number of elderly, multimorbid people. Thus, a comprehensive transformation in work organization as well as corporate management in nursing is of enormous social importance.
12. International efforts
In many regions of the world, there are efforts to introduce a four-day workweek. Iceland, for example, attracted international attention because an experiment with a four-day workweek did not harm productivity. The United Arab Emirates (UAE), which includes the emirate of Dubai, has introduced four-day workweek projects for government facilities and government agencies. The UAE also introduced a new weekend on Jan. 1, 2022. It starts from Friday noon and is extended to Saturday and Sunday. This is associated with a new working time regulation in public authorities, which provides for at least a 4.5-day working week. In future, the working week will start on Mondays and end at 12 noon on Fridays. With the new regulation, Dubai and the other emirates are adapting even better to global markets and also offering citizens and employees an increased balance between work and leisure. The United Arab Emirates became the first country in the world to move away from the five-day workweek. The country is also adapting to the Western weekend rhythm – unlike all its neighboring countries (Spiegel Wirtschaft, 2021).
The four-day week is most advanced in Iceland. Studies in Iceland and the United Kingdom have shown that employee well-being and satisfaction have improved significantly. In addition, work processes were optimized and there was closer collaboration with colleagues. Productivity remained largely the same or increased. In German-speaking countries, the model of the shortened workweek is still the exception (Hotz, M., 2022).
Conclusion on New Work in Healthcare
Attracting and retaining good employees is the fine art of HR management in times of a massive shortage of skilled workers in the care sector. The decisive factor here is knowledge of the change in values in the new working world and the cultural implementation of New Work in HR. There is no question that New Work measures require financial and human resources. In the long term, these investments will pay off in the form of lower complication rates, patient length of stay or fluctuation such as sick days of employees (Dauth T., & Kilz, S., 2022).
With antiquated management methods, hierarchy and “status thinking”, companies do not succeed in being considered an attractive employer for (young) employees. Based on the presented implementation possibilities and recommendations for action, the New Work concept can finally be better understood and realized in care institutions. Feedback culture: constructive feedback supports optimization processes. Open and respectful interaction creates a good basis for trust. Good cooperation releases the courage to take the initiative and the potential for innovation. Time for the development of ideas creates opportunities for testing. The associated tolerance for mistakes ensures self-confidence for self-determined work. Establish and exemplify an open feedback culture at your facility. Give your employees opportunities to develop ideas, test them, fail and grow from them.
Acceptance and training: Change starts with the executives. It is therefore essential that the executives stand behind the decision for a transformation process. For this, comprehensive know-how about the potentials, the challenges explained and also implementation measures is of central importance. But employees must also be involved and informed in the implementation of transformation projects, e.g., through flyers, workshops or an open round of discussions. Build up knowledge in the area of New Work for you and your managers and learn about new forms of leadership. In addition, keep your employees informed and be available for queries.
Regular employee discussions: The decision to take up the nursing profession is closely linked to the social and meaningful tasks associated with it. Talk regularly with your employees about their motivation for pursuing this profession, about their requirements for the current working conditions and about measures to optimize these. Demand analysis: by analyzing (see Gemba Walk) a working day, work peaks can be identified and new working hours and shift schedules (taking into account the required qualifications) can be worked out from this. This can allow for a more flexible approach to the individual needs of employees in terms of work schedules. Conduct a needs analysis for your facility with regard to the necessary resources per time of day and thereby enable your employees to have individualized and needs-based (co-determined) working times.
Digitization of processes: already today, there are numerous technical tools that can be used for work organization in nursing. According to the Fraunhofer Institute IMW, automated processes can create synergies in data collection and optimize care processes with duty scheduling. Digitalized processes can allow more time to work on the patients:inside. Therefore, check which processes can be digitized or automated in your facility in order to relieve employees. Work out the requirements together with the employees. It takes patience. Even if the potential of the measures is not yet apparent in the short term, the effects will become apparent in the long term.
New Working Space: The Bertelsmann Foundation notes in connection with the implementation of New Work: “…not everything is the same for every person, every team, every company, and not everything always has to be new or done differently. The aim is to find the right levers to awaken hidden potential and activate new resources. Hence the organization’s guiding principle: “Humanity before bureaucracy. Unfortunately, traditional care organizations are often far removed from this. The shortage of skilled workers is not the only problem here; there is also, for example, how the few employees are organized. The Bertelsmann Stiftung’s Future of Care project is working to improve working conditions in the care sector.
Probably the best-known example of New Work in care is the Dutch company Buurtzorg (neighborhood). Also under the guiding principle of “humanity before bureaucracy,” Buurtzorg provides a completely new approach to how we can organize care effectively and humanely in a rapidly aging society. At Buurtzorg, caregivers work in small hierarchy-free teams of 4 to 12 people and organize themselves independently within these teams. They decide independently on duty roster, budget and measures. Ideally, the team members come from the same neighborhood and take care of the “neighbors” in need of care. This creates more responsibility, but also room for autonomous and individual organization of the assignments. The focus is on the person in need of care and a caregiver as a reference person. This creates a strong bond between caregiver and patient and an individual care situation that is completely adapted to the needs of the patient. The caregivers are free to organize the care services as they wish. They can provide the services themselves, or they can ask the social environment or spouses to do it for them. This freedom arises from the fact that the caregivers do not charge according to services, but according to hours (time rate). This form of work meets with great approval among both caregivers and those in need of care. Nevertheless, there are also caregivers who do not feel comfortable with this new work concept and the new freedoms right from the start. And that’s quite normal – it’s important to provide good support, offer training, communicate openly and have an open ear for employees. Responsibility, self-organization and acceptance of new ways of working develop first, and this is only possible if there is room for trial and error (Bovenschulte M., et al. 2021).
View of Switzerland: Companies in Switzerland are forced not to wait for the implementation of the policy on the care initiative. Some hospitals have reduced weekly working hours while keeping wages the same.
Profound change: The world of work is undergoing fundamental, technology-driven and social change. This creates new challenges for companies to position themselves as attractive employers. The new workspace environment as well as patient- and employee-centered process design are seen as the answer to the current and future shortage of skilled nursing staff. In addition to the low wage structure, the insufficient compatibility of work and family in shift, on-call and weekend service are the main reasons for not remaining in the profession. But also the low esteem and a rigid hierarchical management with a lack of development prospects and decision-making authority (possibility of participation with a sense of purpose) make nurses consider changing the profession. Not to mention the increasing compression of working hours and tasks with risk of physical, psychological and emotional overload (Dauth, T., & Kilz, S., 2022). The aforementioned characteristics lead to the declining attractiveness of this profession and, as a result, to problems in recruiting new staff with high sickness rates and fluctuation. New Work in nursing offers enormous potential in terms of adjusting screws for this system-relevant industry. New Work helps to identify and use the right levers not only to exploit existing potential, but also to open up new resources and digital support. With this attitude, the work can be made more attractive for the skilled workers who are in demand – and thus the care sector can be positioned for the future (Bovenschulte M., et al. 2021).
A reduced hierarchy in no way leads to a lower or worse economic performance. On the contrary, nurses are more motivated and more willing to perform. The implementation of New Work, decentralization and the reduction of hierarchies do not lead to additional costs in the medium and long term.
Further information is available on request.
Sources and further information
Barmettler, S., Handelszeitung, Was sich ändern muss, Nr. 48, Ringier Axel Springer, Zürich Dezember 2022
Bovenschulte M., Busch-Heizmann, A., Lizarazo López M., Lutze M., Tiryaki S., Trauzettel F., Potenziale einer Pflege 4.0 für die Langzeitpflege – Ergebnisse, Praxisbeispiele, Handlungsempfehlungen, Bertelsmann Stiftung, Gütersloh 2021
Bundesagentur für Arbeit, o.V., „Arbeitsmarktsituation im Pflegebereich“, Berichte: Blickpunkt Arbeitsmarkt Mai 2022
BR24 Redaktion, oV., Pflegeverband warnt vor Kollaps im Gesundheitswesen URL: https://www-br-de.cdn.ampproject.org/c/s/www.br.de/nachrichten/amp/deutschland-welt/pflegeverband-warnt-vor-kollaps-im-gesundheitssystem,TOphoDI, 02.12.2022
Buurtzorg Niederlanden Homepage: Buurtzorg Nederland, URL: https://www.buurtzorg.com/ 2022
Change – das Magazin der Bertelsmann Stiftung „Die New-Work-Innovation in der Pflege: Buurtzorg“, Gütersloh 2020
Dauth T., Likz S. „New Work in der Pflege“ Fraunhofer-Zentrum für Internationales Management und Wissensökonomie IMW, Leipzig 2022
Dovgucic A., URL : https://www.lindera.de/pflegeberuf/new-work-in-der-pflege/ 04.07.2022
Gentner, S. papershift. Von New Work in der Pflege – machbar oder vollkommen unrealistisch?: https://www.papershift.com/blog/new-work-in-der-pflege-machbar-oder-vollkommen-unrealistisch 08.09.2022
Hackl, B., Wagner, M., Attmer, L. & Baumann, D. Auf dem Weg zur neuen Arbeitswelt: Management-Impulse, Praxisbeispiele, Studien“ Springer-Verlag, New Work 2017
Hentl-Merget, J. „Vertrauen statt Kontrolle“, CNE Pflegemanagement, Ausgabe 01/2020, Seiten 4-6, 2020
Hermann, M., John, A., Wenger, V., CSS Gesundheitsstudie Sotomo, 2022
Hofmann, J., & Günther, J. (01. 08 2019). Arbeiten 4.0 – Eine Einführung – Working in the Digital Age. HMD Praxis der Wirtschaftsinformatik Volume 56., S. 687-705
Hotz, M., Handelszeitung Nr. 44, Management: Vier-Tage-Woche im Test, Zürich 03.11.2022
Jonsdottir, E. Medinside. Von Personalsuche Italien, Winterthur 08. 11 2022, URL: https://www.medinside.ch/personalsuche-italien-%C2%ABwie-sind-die-reaktionen-aus-der-branche,-herr-blasi%C2%BB-20221108
Kircher D. S., New Work and Retention Management in the Health Sector – A Response to the Staff Shortage in the Healthcare Sector, Zürich 2022, URL eigener Artikel: https://morethandigital.info/en/new-work-and-retention-management-in-the-health-sector
Korte, L., & Bohnet-Joschko, S. Digitization in Everyday Nursing Care: A Vignette Study in German Hospitals. International Journal of Research and Public Health, MDPI, S. Int. J. Environ. Res. Public Health 2022, 19, 10775, 13 Seiten, Witten 30. 08 2022
Krüger, R., Becker, W., Groening, A., Tollmann, F. J., Keck, C., Lean Management im medizinischen Labor – Mehr Qualität und Effizienz, Trillium Diagnostik, Band 20, Heft 1, Grafrath 2022
Mahlodji, A. Next Level WORK – Eine Anleitung zum mutigeren Arbeiten.: Zukunftsinstitut GmbH, Frankfurt am Main 2021
Ohanian, M., 15-Stunden-Woche: Warum sich Keynes so massiv irrte, Handelszeitung, Ringier Axel Springer Schweiz AG, Zürich 2016, URL: https://www.handelszeitung.ch/blogs/free-lunch/15-stunden-woche-warum-sich-keynes-so-massiv-irrte-1037721, Zugriff 26.12.2022
Redel V., PFLEGESENSITIVE INDIKATOREN, Care Solutions, URL: https://www.pflegeinformatik.at/pflegesensitive-indikatoren/ St. Veit 08.1.2021
Reichl V., Pflegeintervention und Pflege-Outcome, Hamburger Fern-Hochschule Studienbrief, Hamburg 2017, URL: https://www.studocu.com/de/document/hamburger-fern-hochschule/pflege-im-prozess/4-pflegeintervention-und-pflegeoutcome/3927965
Ribi, Y. SBK, ASI. Die Stimme der Pflege: 09.03.2018, URL: https://www.sbk.ch/aktuell/news-single?tx_news_pi1%5Bnews%5D=58&cHash=67da0f5f8baf800f0c87e08826cb6092
Steinbeck, V., Ernst, S.-C., Pross, C., Patient-Reported Outcome Measures (PROMs): ein Internationaler Vergleich – Herausforderungen und Erfolgsstrategien, Bertelsmann Stiftung, Gütersloh 2022
Tschudy, D. Handelszeitung Nr. 46, Die grosse Kunst der Motivation, Zürich 17.11.2022

Comments are closed.