“New Healthcare Management” The Digital Health Revolution
An Approach to Successful Healthcare Transformations
The goal is clear – the path and the speed to take are not: The (digital) transformation of the healthcare system in the German-speaking countries (Germany, Austria, Switzerland, and Liechtenstein) is progressing rather slowly. Using Switzerland as an example, this article examines the root causes, useful best practices, and the contribution managers can make by following the New Healthcare Management approach.
Is digital health revolutionizing healthcare? Nobody really knows. What we do know is that health policy decision-makers will be faced with numerous major demographic and technological challenges over the next ten years. Coupled with an increased cost burden, these challenges, will put immense pressure on them to initiate change.
We all want quality health care that considers the needs of individual patients while remaining affordable. A positive development we can observe in German-speaking countries is the arrival of digital solutions in the public healthcare discussion. For example, the Swiss Federal Council’s “Swiss Health Policy Strategy 2020–2030” outlines the vision of a digital, high-quality, and financially sustainable healthcare system by 2030 [1]. Such centralized visions can serve as a guide rail for the transformation of our systems.
As practitioners and health economists, we need to embrace the vision, work on concrete approaches, and ensure that our system is viable in the long term. For the transformation of the health system to succeed, we must have a thorough understanding of digital health in its very essence – and apply this knowledge effectively. Against this background, the question arises whether an individual actor can contribute anything to the transformation of the whole system.
This article, therefore, takes Switzerland as a case study and assesses its digital health maturity. In addition, we discuss the extent to which individual healthcare executives can make a contribution to the (digital) transformation by following the “New Healthcare Management” approach and promoting it among their employees.
Index
The Current Status of Digital Health – Using the Example of Switzerland
In my previous post (in German), I discussed the term digital health in detail. The key message was that digitalization is not a process that can be promoted independently without considering other structural issues of our healthcare system. Digitalization only makes sense when all players in the healthcare network are taken into account.
A country-by-country comparison is always helpful when evaluating the digitalization of a national healthcare system. In the case of Switzerland, international comparisons paint a bleak picture of its digital maturity level. For example, a study conducted by the Bertelsmann Foundation in 2018 shows a large number of countries outranking Switzerland in the field of digitalization [2], with Switzerland ranking 14th among 17 countries. As a small consolation prize for simple minds, its eternal rival Germany was two places behind.
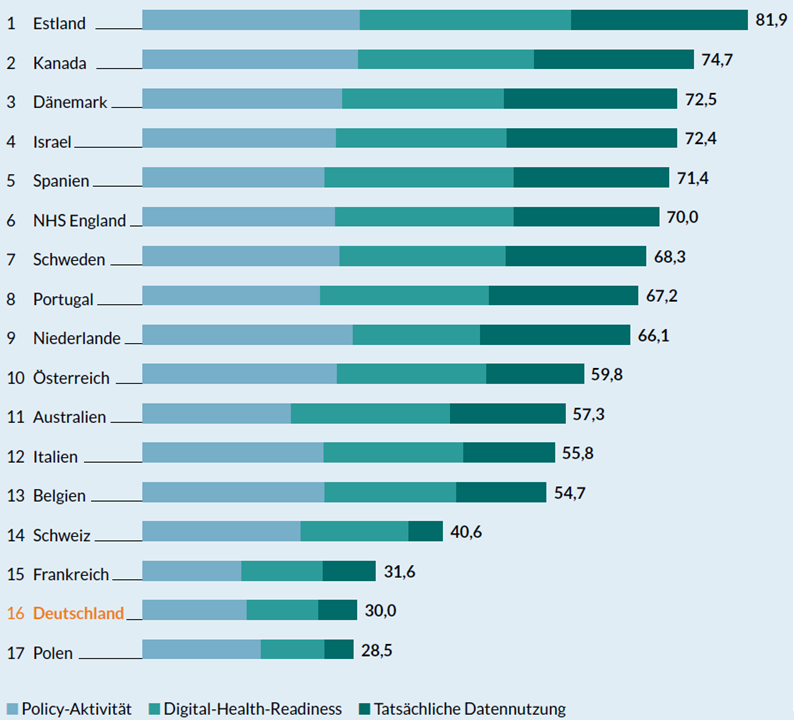
The dynamics of such international comparisons need to be considered as well, however. No one can be sure that the ranking will stay the same. For example, Germany has experienced a strong digitalization drive in recent years. A large number of legal changes have been initiated. A news headline recently pointed out the astonishing speed of this transformation: 34 laws passed in 32 months! (“34 verabschiedete Gesetze in 32 Monaten” (…)). In fact, Germany may well have overtaken Switzerland by now.
It would be interesting to know why the Swiss health care system has been given such a low ranking. From my perspective, there is not just one reason to explain this, but rather a combination of factors.
- One such factor is the very slow implementation of national digital health services such as electronic patient records (Switzerland’s EPD is the equivalent to Germany’s ePA), telemedicine, and electronic vaccination records. This slow implementation level is even more astonishing in the light of Switzerland’s prosperity and small size, both of which should provide a good basis for rapid digitalization. Countries such as Estonia and Denmark, which are at the top of the ranking, are good examples of this.
- It turns out, however, that the fragmentation caused by the Swiss federal system inhibits rapid digital transformation. Because the 26 Swiss cantons are entitled to issue their own regulations on many issues, it is difficult for service providers, insurers, and other private healthcare providers to interpret and fulfill these requirements correctly. Despite the requirements issued at the federal level, there remain uncertainties and opposing incentives. The introduction of the EPD, for example, was delayed several times, and the private digital vaccination passport platform meinimpfungen.ch had to be shut down due to serious security problems, locking out the data of hundred thousands of citizens.
Overall, does this mean that there is little hope for a successful digital transformation of our healthcare system? Not quite. On second glance, despite setbacks, there are also many innovative digitalization initiatives in the Swiss system that are encouraging.
Digital Heath in Switzerland – Good Practices
The current Digital Health Report 2021/22 [3] records the digital health developments during that period. The coronavirus and the measures to prevent its spread have become a driver of digitalization in many industries. The COVID-19 pandemic has forced the Swiss health system to adopt new approaches. The Swiss Medical Association FMH now provides its members with a free tool for carrying out telemedicine consultations via video [4]. The multitude of digital interim solutions during the pandemic also presented the authorities with challenges: On the one hand, they had to carefully evaluate digital health applications and, on the other hand, implement them as rapidly as possible as part of the pandemic response plan.
“Digital health solutions can create conditions that enable faster and more targeted decisions. However, there are always setbacks in implementing them.”
Established Swiss telemedicine providers such as Medi24 and Medgate have reported impressive growth rates at the beginning of the pandemic [5]. The digital health subsidiary of Swiss insurer Santé24 provides its customers with the TytoHome telemedicine device, which can be used to carry out many examinations at home, including throat swabs. The data collected can then be discussed directly with a santé24 medical specialist via video chat [6]. At the same time, despite the fragmentation described, more and more players are forming alliances to initiate a bottom-up digital transformation [7]. Examples in Switzerland include, among many others, the Swiss Digital Health Roundtable, and CH ++.
My conclusion is that healthcare digitalization is advancing slowly but steadily – regardless of our fragmented health system and without waiting for a major strategic initiative by the central government. Healthcare players are continuously implementing innovative digital health solutions, putting them in the driver’s seat.
The (obvious) secret of successful transformation – cultural change!
You may wonder what unites the case studies of successful digital health transformation. The good practices we analyzed are not the result of technological breakthroughs. The digital transformation of our healthcare system is much more than just a technology project. It takes will and perseverance, and especially a change in the organizational culture. Positive results have been achieved where people have consciously sought progress. Numerous organizations have recognized this and are pushing ahead with their digitalization initiatives. They are adapting their strategy iteratively, setting up innovation departments in their organizational structures, and systematically carrying out pilot projects.
“The digital transformation of our healthcare system is much more than just a technology project. It takes will and perseverance, and especially a change in the organizational culture.”
Policy-makers and decision-makers in society must now promote this innovation potential, learn from past mistakes, and spread the good news of successful initiatives. My job as a health economist must be to support practitioners in their digital transformation. In addition, I am convinced that a digital health approach cannot stand on its own – a fundamental change is required in our health system to enable it to cope with the upcoming challenges that have been identified. Practitioners have to decide which conceptual models they will follow in designing their organizations and how to run them in a modern way.
Your contribution: Be a “New Healthcare Management” leader!
What small contribution can each individual make as part of an overall health system? My answer is: Rethink your leadership style and your organization! The ideas behind the New Healthcare Management approach may help here [7]. In my approach, I proposed seven management concepts that, in my opinion, can make a major contribution to the further development of our health system: positive leadership, value-based healthcare, design thinking, Lean & Kaizen, self-organization, agility, and, of course, digital health. Although they are used individually by many organizations, they are highly interdependent and usually complement each other very well.
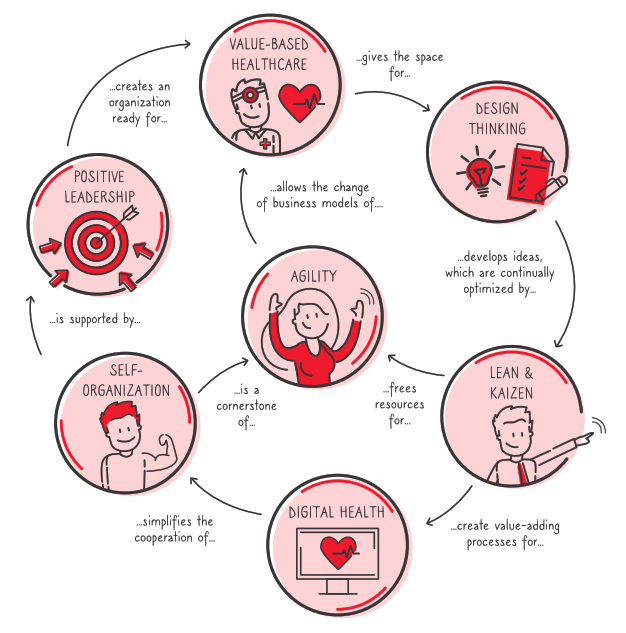
Even if the transformation of your team or organization will not suddenly lead to a revolution of the overall system: Business history has repeatedly shown how individuals became beacons of light with their good practices and inspired others as role models. Indirectly, they have an impact on the overall system. I see two options for you, the reader of this article: You can continue to complain about “those up there doing nothing” – or you can use your own sphere of influence and make a contribution to a better health system following the New Healthcare Management approach by changing yourself and your team.
If we manage to create enough best practice examples and convince the public of the advantages of a digital healthcare system, politicians will follow and create the appropriate legal framework. The international best practices show that there is justified hope for a transformation of our system. We can start to change voluntarily before the external pressure becomes so high that the transformation becomes mandatory. So why not start today?
“Paths are created by walking” – Franz Kafka
Bibliography
[1] Bundesamt für Gesundheit (2020). Die gesundheitspolitische Strategie des Bundesrates 2020–2030. Bern
[2] Kostera, T., & Thranberend, T. (2018). #SmartHealthSystems – Digitalisierung braucht effektive Strategie, politische Führung und eine koordinierende nationale Institution (Nr. 5; Daten, Analysen, Perspektiven). Bertelsmann Stiftung
[3] Angerer, A., Hollenstein, E., & Russ, C. (2021). Der Digital Health Report 21/22: die Zukunft des Schweizer Gesundheitswesens. ZHAW Zurich University of Applied Sciences. https://doi.org/10.21256/ZHAW-2408
[4] Enz, K. (2020, April 24). Digitalisierung im Gesundheitswesen: Coronavirus wird zum Treiber. St.Galler Tagblatt AG. Retrieved from https://www.tagblatt.ch/wirtschaft/corona-beschleunigt-die-digitalisierung-im-gesundheitswesen-ld.1215109
[5] Medinside (2020, June 26). Telemedizin legt in Coronakrise deutlich zu. Retrieved from https://www.medinside.ch/de/post/telemedizin-legt-in-coronakrise-deutlich-zu
[6] Amelung, V., Ex, P., Hildebrandt, H., & Knieps, F. (2020). Nachmachen erlaubt: Innovative Ansätze aus dem Schweizer Gesundheitssystem. Gesundheits- und Sozialpolitik (G&S), 74(6), 42 – 48. https://doi.org/10.5771/1611-5821-2020-6-42
[7] IG eHealth. (2021, März 31). Gesundheitsverbände gründen Allianz «Digitale Transformation im Gesundheitswesen». Retrieved from: https://www.ig-ehealth.ch/2021/03/31/gesundheitsverb%C3%A4nde-gr%C3%BCnden-allianz-digitale-transformation-im-gesundheitswesen/
[8] Angerer, A. (ed.) (2021). New Healthcare Management (1st ed.). Berlin: Medizinisch Wissenschaftlicher Verlag

Comments are closed.